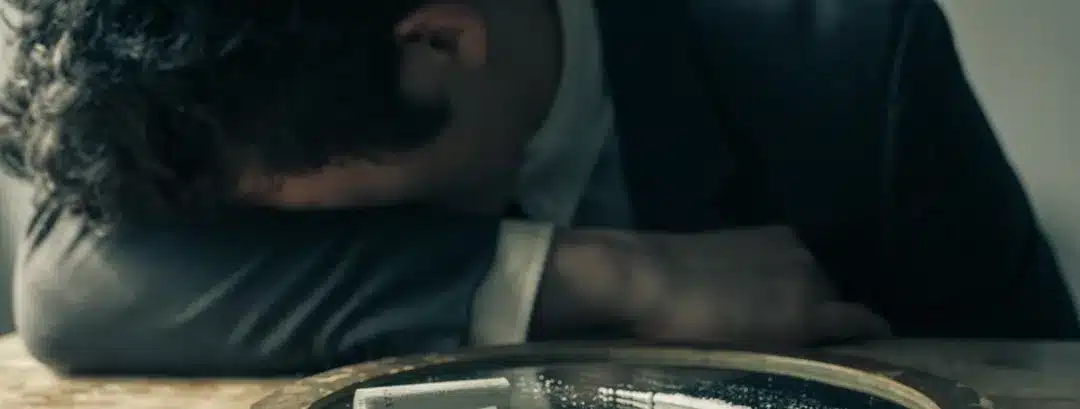
Looking at Healing from Cycles of Cocaine Use and Bipolar Disorder
Bipolar disorder is known for its high periods of mania and low periods of depression. While manic periods can make a person feel happy and euphoric, the lows can be incredibly overwhelming.
Often, a person might try to do what they can to get out of this depressive period, including using uppers like cocaine. This is why co-occurring bipolar and cocaine use disorder is a common diagnosis.
If you or a loved one are struggling with bipolar and cocaine abuse, you have found the right resource!
Even though cocaine use can temporarily make you feel better because of its effects on serotonin in the brain, eventually you will come down from that high. This can make depression worse. Cocaine abuse also makes it more challenging to treat bipolar disorder, however, recovery is possible.
Keep reading to learn more about the bipolar-cocaine connection, how cocaine affects your brain, diagnosing bipolar, and how Purpose Healing Center can help you take those early steps toward treatment.
The Link Between Bipolar and Cocaine Addiction
According to the National Comorbidity Survey, individuals with bipolar disorder have an increased risk of co-occurring substance abuse, including alcohol, marijuana, and cocaine. In one study, 20% of patients with bipolar also admitted to abusing cocaine. Cocaine and crack cocaine use is also higher in patients with bipolar than it is in the general population.
Often, people with bipolar turn to stimulant abuse because of the euphoric effects on the brain. However, while it can improve mood in the short term, it also causes dopamine to rush to your brain. After you’ve stopped using the drug, you will crash. With dopamine levels being burnt out, it can even make depression worse than it was before.
This creates a harsh cycle. You may even develop stimulant dependence, meaning that you need to use cocaine to feel “normal”.
Additionally, individuals who have co-occurring cocaine use and bipolar disorder are less likely to follow through with treatment for both diagnoses. It is not uncommon for bipolar clients to stop taking medication and going to therapy when they feel “better” in between episodes or during a manic period.
How Cocaine Interacts with the Body and Brain
After cocaine use, most people experience enjoyable side effects. Cocaine raises levels of dopamine in the brain, making you experience feelings of happiness and euphoria. It increases energy levels, makes you feel more confident and social, and lowers inhibits and decision making similar to the way that drinking alcohol does.
Additionally, cocaine interacts with the pleasure center of the brain, making you feel good about things. These feelings of euphoria and happiness are one of the reasons someone with bipolar disorder might use cocaine when they are feeling depressed.
Unfortunately, this begins a vicious cycle. The happy feelings associated with cocaine use only last for so long. Dopamine levels come crashing down and it can cause you to feel even more depressed than you did before using the cocaine.
What is Bipolar Disorder?

Bipolar disorder, or manic depression, is characterized by cycles of manic and depressive episodes. During manic episodes, you may feel full of energy, hyper, or euphoric. When experiencing depressive symptoms, you may feel sad or hopeless and withdraw from activities.
How these cycles present and the specific symptoms you’ll experience can vary slightly.
7 More Common Types of Bipolar Disorder
One of the challenges of diagnosing bipolar disorder is that there are several types. In addition to symptoms of depression and mania, individuals with bipolar spectrum disorder can experience anxiety, melancholy, and psychosis.
Bipolar I and Bipolar II are the main types of bipolar disorder, however, it can be classified using other categories. Notable characteristics of the different types include:
1) Cyclothymic Disorder
If you have experienced more than one manic and depressive episode over 2 years, you may be diagnosed with cyclothymic disorder. While this is not considered as severe as bipolar I or II, you can still experience symptoms and need treatment. Additionally, having this type of bipolar disorder increases the risk of a diagnosis of bipolar I or II and other psychiatric disorders in the future.
2) Bipolar I Disorder
If you have bipolar I disorder, you may experience at least one manic episode each year. This type of bipolar has manic features and while some people have depressive episodes too, not everyone does. Typically, you return to a period of hypomania or depression in between manic episodes.
3) Bipolar II Disorder
Bipolar II disorder is characterized by having at least one major depressive episode, followed by a manic period that lasts at least four days. If you are diagnosed with Bipolar II, you often return to a period of “normalcy” between depressive episodes. It’s also more likely that you have comorbid diagnoses including alcoholism, substance abuse, and anxiety disorders.
4) Bipolar with Seasonal Patterns

Individuals with this type of bipolar disorder have symptoms of either Bipolar I or II. However, extreme mood swings associated with bipolar are likely to be affected by the seasons.
5) Bipolar with Mixed Features
This type of bipolar is characterized by mixed episodes of depression and mania. Some people experience episodes rapidly, while others experience depressive and manic symptoms at the same time.
6) Rapid Cycling Bipolar
You may have rapid cycling bipolar disorder if you have more than 4 episodes of mania, depression, or mixed symptoms each year. With this specific mood disorder, it can be weeks between episodes and the length of each episode can vary. They can last days, weeks, or months.
7) Unspecified Bipolar Disorder or Bipolar NOS
In the case of unspecified bipolar mood disorder, you may not meet the exact criteria for other bipolar diagnoses. However, it’s worth noting that does not mean you do not need help.
Additionally, bipolar disorder is only one of the psychiatric disorders with mood swings, depressive episodes, and manic episodes as the primary symptoms. To get a definitive diagnosis, you’ll need to schedule with a psychiatrist. They may diagnose bipolar or another co-occurring disorder.
One of the benefits of attending rehab at Purpose is that we are a dual diagnosis center. This makes it easy to get a diagnosis and receive mental health treatment while you are already attending rehab for substance abuse treatment.
What are the Symptoms of Bipolar Mania?

The “high” periods associated with bipolar are labeled mania or hypomania. Manic symptoms that a person with bipolar might experience include:
- Increased energy levels and activity
- Feeling abnormally upbeat or talkative
- Jumpiness or agitation
- Racing thoughts
- Difficulty paying attention
- Needing less sleep than usual
- Feeling euphoric or overly confident
- Poor decision making including promiscuity, spending money, gambling, risky behaviors, etc.
A manic episode is considered more intense than a hypomanic episode. Individuals who are manic are more likely to require hospitalization after experiencing psychosis.
Depressive Symptoms of Bipolar
During the “low” periods associated with bipolar, some of the most common symptoms are:
- Sleeping too much or not enough
- Unintentionally losing weight from poor eating habits
- Loss of energy and fatigue
- Difficulty thinking and making decisions
- Feeling sad and empty
- Crying spells
- Feeling hopeless or helpless
- Difficulty feeling pleasure
- Isolating tendencies
- Self-harm
- Suicidal thoughts, plans, or attempts
According to the American Psychiatric Association, at least five of these symptoms must be present for it to be considered an episode. Often, depressive symptoms are so severe that they interrupt your ability to function in day-to-day life.
Can Using Drugs Cause Bipolar Disorder?
While it is not known if abusing cocaine or other illicit substance abuse causes bipolar disorder on its own, according to the National Institute of Health, substance use disorders worsen the onset of bipolar. Furthermore, the symptoms of bipolar disorder may be worse in substance users.
While cocaine abuse or alcohol abuse can affect the onset of bipolar disorder, it is not known what exactly causes it. However, it is known that individuals who have certain genes are more likely to be diagnosed with bipolar disorder and it tends to run in families. It is likely caused by genetics, but certain environmental factors can also contribute to the severity of symptoms.
How Do I Know if I’m Addicted to Cocaine?

Often, a person becomes addicted to cocaine after using it recreationally a few times. They enjoy the way that it makes them feel and over time, use becomes more frequent. This can even seem “normal” depending on your social circle.
Even though the signs may be there, substance abusers sometimes need concrete evidence that substance use is negatively impacting their lives to motivate them to take the first step to quit. Some signs that you have a substance use disorder include:
- Experiencing depression after a binge cycle
- Developing a tolerance, needing more cocaine to feel the same “high” as before
- Marked mood symptoms and mood swings not caused by bipolar disorder
- Increased alertness, talkativeness, and energy
- Lying about drug abuse to concerned family or friends
- Withdrawing from sober friends and loved ones
- Experiencing withdrawal symptoms after quitting cocaine
- Engaging in risky behaviors that you wouldn’t engage in if sober
- Facing financial, legal, or relationship problems due to cocaine use
- Using cocaine with another drug, alcohol abuse
While drug abuse counselors at other facilities can diagnose cocaine addiction and co-occuring alcohol dependence, they may be less aware of bipolar depression or other co-occurring disorders. Diagnosing co-occurring cocaine dependence is important for full recovery.
If you treat cocaine withdrawal and dependence without also addressing underlying mental illness, there is a greater risk of relapse, which is why at Purpose Healing Center, we seek to address the root causes of drug use and abuse.
Knowing the Risk Factors for a Cocaine Use Disorder
Use of stimulants, amphetamines, alcohol, and other drug abuse is more common in clients with co-occurring bipolar disorder, antisocial personality disorder, and other mental disorders. However, this is not the only risk factor for cocaine addiction. Often, it is thought that cocaine dependence is caused by a combination of genetic and environmental risk factors.
Some environmental risk factors associated with cocaine use include socioeconomic factors, social media and peer pressure, and childhood adversity and trauma. Other factors that cause an increased risk of cocaine addictive disorders include psychological factors like underlying mental disorders or thrill-seeking behavior.
Finally, a person’s gender, ethnicity, genes, and stage of development may also contribute to an increased risk of cocaine dependence.
Effective Treatment Options for Cocaine and Bipolar

In individuals who have bipolar with comorbid substance abuse, it’s essential to treat both conditions. If you do not treat both affective disorders, it’s unlikely that you’ll maintain long-term sobriety. At Purpose, we approach bipolar and co-occurring substance use disorders individually but at the same time.
To do this, we’ll work with you to create a comprehensive bipolar disorder treatment plan unique to your specific diagnosis.
Inpatient vs Outpatient Treatment for Bipolar and Cocaine Abuse
Many clients with co-occurring bipolar and substance abuse start with inpatient treatment. The length of an inpatient treatment plan depends on your specific needs and may last 30, 60, or 90 days. At Purpose, inpatient treatment includes medical detox, physical activities, group therapy, individual therapy and psychiatric care, and music, art, and other alternative therapies.
It is also not uncommon for individuals seeking treatment for bipolar and substance-related disorders to start with inpatient treatment and then transition to outpatient treatment. Immediately after rehab, this might involve attending a partial hospitalization program, intensive outpatient program, or sober living facility.
Programs like these provide extra support right after rehab when the risk of relapse is the highest. they can be a useful tool for individuals with bipolar disorder and cocaine dependence.
From there, most clients continue seeing a psychiatrist, taking psychiatric medications as prescribed, and working with an individual therapist. Many people with cocaine addiction also attend Narcotics Anonymous meetings in their local area. This is a useful resource for building support and talking about drug use and mental health problems with people who understand the challenges of staying sober.
The Importance of Dual Diagnosis Treatment
Clinical trials on evidence-based therapies and effective treatments for chronic drug use show that when a person has co-occurring substance use disorder and mental illness, it’s important to address both problems during drug addiction and bipolar disorder treatment. At Purpose Healing Center, our staff are trained in dual diagnosis care.
By treating bipolar symptoms in addition to addressing drug abuse, there’s a greater chance of relapse prevention. This is especially important for bipolar disorder patients who may have addictive tendencies as a result of their mental health condition.
During dual diagnosis treatment for individuals who abuse drugs with co-occurring mental health concerns, medication may be prescribed to manage bipolar symptoms. Individuals with bipolar also often benefit from cognitive behavioral therapy.
According to the clinical definition, this type of therapy focuses on identifying unhelpful thought patterns, managing emotions without reacting to them, and improving poor decision-making and behaviors associated with mood disorders.
Do I Need to Take Medication if Have Bipolar Disorder?

Bipolar disorder is a lifelong (chronic) condition, much like drug addiction is considered a chronic relapsing disorder. Often, medication is prescribed to manage the symptoms of different bipolar disorders.
Some of the most common medications prescribed include mood stabilizers, antidepressants, antianxiety medication, and antipsychotics. Psychotherapy is also very beneficial for those seeking relief from the symptoms of bipolar disorder.
In addition to being a chronic condition, bipolar is a serious mental illness. Many people do need to take medication throughout their lives to manage their mental health. Even though there may be periods when you feel better, it is still important to continue taking medication as prescribed.
Get Help Overcoming Co-Occurring Disorders at Purpose
Bipolar and substance use disorders are hard enough to overcome individually. When you are diagnosed with both, it presents unique challenges. Fortunately, at Purpose Healing Center, we are ready to rise to that challenge to help you improve your mental health as you begin on a path to lasting recovery.
Even if you’ve tried other rehab facilities in the past, most do not offer the same level of care that you’ll find at our Joint Commission Accredited treatment center. We will be with you through every step of the process, from verifying your insurance and arranging transportation to our facility to deciding on the best course of treatment for your co-occurring disorders.
No matter how bipolar disorder and cocaine use are affecting your life, you can find the support you need to overcome it at Purpose. Make the confidential call now, and get our help today!
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8623998/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2094705/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851032/
- https://www.mayoclinic.org/diseases-conditions/bipolar-disorder/symptoms-causes/syc-20355955
- https://pubmed.ncbi.nlm.nih.gov/7883738/
- https://www.nimh.nih.gov/health/publications/bipolar-disorder